The opioid crisis is one of the largest public health emergencies in the United States and a growing global concern as opioid overdoses affect communities worldwide. Some countries have implemented decriminalization policies and treatment practitioners are desperate for innovative solutions to this substantial crisis. Ibogaine for opioid use has historically provided relief to many suffering from opioid abuse disorders. Could this African shrub root extract provide aid to this vulnerable community? Let’s explore ibogaine for opioid use disorder and how the roots of African ceremonial traditions transform the lives of people battling substance use disorders.
What is Ibogaine?
Ibogaine is a naturally occurring psychedelic alkaloid derived from the bark of the African shrub Tabernanthe iboga—colloquially referred to as iboga. This perennial shrub grows abundantly in West and Central Africa, where indigenous groups discovered and utilized the ibogaine extracts in religious sacraments, coming of age traditions and healing ceremonies. Researchers believe that native groups—specifically the Pygmy and Bwiti tribes—used low doses of ibogaine to fight against fatigue, hunger and thirst, while high doses served to instigate intense visual hallucinations, often reported as connections with ancient intergenerational wisdom and divine spirits.
Biological Perspective
Researchers are unclear on all of the ways that ibogaine interacts with the brain’s neurological signaling systems. They have found evidence of ibogaine’s effect on neurotransmitter transporters as well as glutamate receptors, nicotinic receptors and opioid receptors.
Glutamate is a major excitatory neurotransmitter that acts as a key: opening ion channels and allowing neurons to send and receive messages.
Nicotinic receptors interact with the neurotransmitter acetylcholine as well as outside chemicals like nicotine. Similarly, opioid receptors—which exist across all nerve cells—interact with naturally occurring endogenous opioids as well as synthetic opioids. This interaction poses intriguing possibilities for ibogaine as a treatment for various forms of substance abuse disorders.
Another mechanism involved in behaviors that mimic substance abuse disorders is the neurotransmitter serotonin and the nucleus accumbens.
Ibogaine and serotonin both have an indole ring structure, allowing ibogaine to bond to serotonin transporters and increase levels of serotonin in the nucleus accumbens. The nucleus accumbens is located in the lower front of the brain—referred to as the basal forebrain—and is an essential area involved in the neural coordination of motivation and action. Habitual substance use disorders behaviors rely on the nucleus accumbens to perpetuate patterns of action. As the brain becomes accustomed to an outside substance the plasticity of the nucleus accumbens diminishes, presenting a predictable pattern of motivation and action.
Though more research is necessary to understand the exact biological mechanism underlying these effects, ibogaine has historically shown promise as a treatment for opioid use disorders.
History of Ibogaine and Opioid Use Disorders
Though indigenous African communities have long experienced the benefits of ibogaine for countless generations, Western researchers and medical practitioners began exploring this shrub root until the early 1900s. Though it was first explored as a neuromuscular stimulant, over the following decades, researchers investigated ibogaine’s potential cardiovascular benefits before discovering its properties that help with substance use in the 1960s. Through animal trials, researchers discovered that when they administered ibogaine to opioid addicted rodents, the animals exhibited fewer withdrawal symptoms and were less likely to continue self-administering opioids over the following weeks. A similar phenomenon was anecdotally occurring in humans, highlighted by the ibogaine treatment pioneer Howard Lotsof.
Howard Lotsof
In 1962, Howard Lotsof was a teenager living in the Bronx and regularly using heroin. One evening a friend of his offered him ibogaine and after a long psychedelic trip, Lotsof found that he no longer experienced heroin cravings and that he felt no withdrawal symptoms. Inspired, he administered ibogaine to a number of his people suffering from heroine use disorders friends and saw similar changes in symptoms, as well as an overall shift in their understandings of substance use. Anecdotally, ibogaine allowed people to see the root causes of their suffering, freeing them to change their perceptions of their substance use—all without the physiological panic of drug withdrawal.
After Lotsof married his lifelong partner Norma in 1964, he continued his education at NYU eventually working in the television and film industry. In 1970, the United States Congress ratified the Scheduled Substance Act which outlawed a number of psychedelic substances, instigated a crackdown worldwide and listed ibogaine—as well others—as a schedule one narcotic with no available therapeutic uses and high probability for abuse.
Despite this, in the 1980s Lotsof continued his investigation of ibogaine as a potential treatment for substance use disorders. In 1985, he acquired a US patent for ibogaine as a clinical treatment for acute substance use disorders. Lotsof also traveled to the equatorial African country Gabon, where the then-president Omar Bongo personally presented him with iboga as Gabon’s “gift to the world.”
Lotsof’s career blossomed over the following decades. He established a research initiative on ibogaine’s related compounds and eventually obtained FDA approval for clinical trials looking into ibogaine for opioid use disorders. He and his wife Norma participated in the first International Ibogaine Provider and Facilitator Conference in 2009, creating a global network of ibogaine treatment facilities. Not only has ibogaine shown promise for opioids but also nicotine, cocaine and alcohol abuse disorders.
The potential of ibogaine as a treatment for opioid use is extremely promising, as over 62 million people worldwide suffer from opioid abuse disorders. Let’s take a look into the ongoing opioid crisis and how ibogaine can help.
The Opioid Crisis
The opioid crisis is an evolving public health phenomenon that is ravaging lives across the globe — particularly in developed countries like the United States. A key component of this growing epidemic is the increase in the public’s access to prescription opiates, as well as the prevalence of synthetic opioids like fentanyl. Though heroin and fentanyl account for most opioid overdoses, a majority of people struggling with opioid abuse begin their substance use disorder with legally prescribed opioids. Chronic postoperative pain occurs in anywhere from ten to fifty percent of patients and is of great concern to the medical community.
Opioids boost pleasurable neurotransmitters and endorphins in the brain, numbing paint and generating an overall sense of ease. This is why they are so helpful in medical intervention but also what makes them so easy to abuse.
Over time, opiates slow the natural production of endorphins presenting as a tolerance. The same dose that was providing the positive feelings now must be increased in order to have the same effect. When the prescription runs out, many turn to illegal opioids like heroin and increase their chances for overdose. In order to help the millions of people struggling with these powerful and destructive substances, recovery practitioners need innovative treatment techniques.
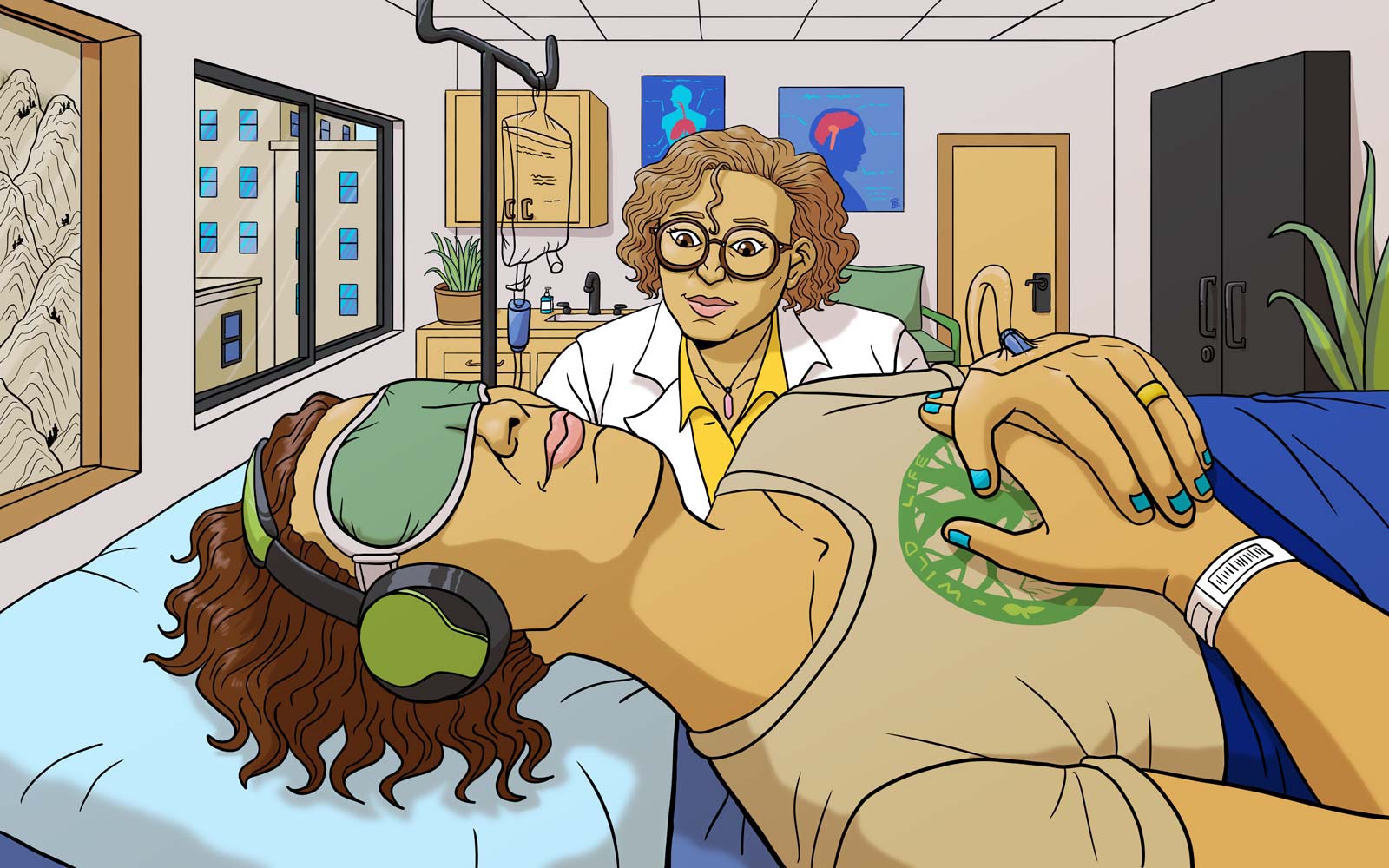
Ibogaine for Substance Use Disorders
Just as Howard Lotsof witnessed with his friends in New York, research continues to show ibogaine’s benefits for opioid abuse disorders. Improvements seem to be most persistent during the month following treatment with residual benefits up to a year after. After their ibogaine treatment, research participants exhibit fewer withdrawal symptoms and report a “slide show” of autobiographical memories that alter their perceptions, forcing them to confront the root cause of suffering behind their opioid use disorder. Researchers believe that one of the long term benefits of this treatment is the changed perspective, allowing participants to improve interpersonal relationships, therefore giving them more support and room to work towards recovery. One subject of a 2017 study reported:
“Iboga will not do the work for you. However, it will help you do your own work.”
Opioid abuse is sometimes mischaracterized in a way that demonizes those struggling with opioid abuse disorders. Supporting communities entangled with substance use promotes healing and can save individuals and families from the prolonged anguish of opioid use disorders. The ancient wisdom accessed through iboga medicine in Africa now has the possibility to change lives across the world and work to heal the scars of the opioid crisis.
Have you ever heard about ibogaine for opioid use? We would be stoked to hear your comments below. If you are interested in learning more about psychedelic medicines, make sure to subscribe to our newsletter.