Ketamine was discovered in 1962. It got its start as a surgical anesthetic used to treat soldiers in Vietnam and was considered relatively safe in comparison to other drugs at the time. Over the past 50 years, ketamine has gone from a surgical anesthetic to a popular veterinary anesthetic, pain reliever and sedative. Presently, doctors are using ketamine treatments to combat treatment-resistant depression in humans. Also, it is often used recreationally as a potentially potent psychedelic. In March of 2019, the FDA approved the S(+) stereoisomer of ketamine, called esketamine, as a fast-acting antidepressant. It relieves the symptoms of depression within four hours of use, and this can last for up to several weeks. However, there can be side effects associated with the ketamine comedown.
Before using ketamine for any purpose, it’s essential to understand how it works in the brain, what the trip itself is like, and how to prepare for the ketamine comedown. For more information on ketamine itself, check out our ketamine guide. For now, let’s dive in and explore a ketamine comedown.
Ketamine in the Brain
Ketamine is an NMDA receptor antagonist, causing it to act as a dissociative anesthetic. While the ketamine dosage, method of consumption and individual body chemistry all play a significant role in its effects, there are several possible outcomes of using ketamine. Common effects of ketamine include inducing a trancelike state, pain relief, sedation, memory loss, euphoria, dissociation, auditory and visual hallucinations from high doses, agitation, confusion, elevated blood pressure, muscle tremors and larynx spasms.
As mentioned, ketamine is becoming a well-known option for the treatment of depression, a common mental health condition. While many antidepressants target a “monoamine” neurotransmitter, such as dopamine or serotonin, ketamine targets glutamate receptors. Glutamate is the nervous system’s most common and abundant excitatory neurotransmitter. It regulates the brain’s ability to process emotions and cognitive thoughts and enhances synaptic connections and neuroplasticity. It is a vital component in how a human responds to experiences in her environment, and how she will learn from and remember these experiences.
Glutamate produces and regulates gamma aminobutyric acid (GABA), an inhibitory neurotransmitter whose primary role is to reduce excitability and promote calmness in the nervous system. If a person has high levels of glutamate and low GABA, he might experience anxiety. Alternatively, low levels of glutamate and increased GABA lead to depression.
Ketamine Use in a Clinical Setting
When ketamine is administered in a clinical environment, there are three phases observed in the treatment. The goal is to strike the right balance of glutamate and GABA to restore balance in the brain and grow new neural receptors. The phases of effects are as follows:
- Immediate effects: Ketamine gets to work quickly by engaging the brain’s opiate receptors. Patients will feel more relaxed and sedated, finding immediate relief from pain and experiencing lessened feelings of depression.
- Continuous effects: Glutamate receptors are working to restore normal levels of glutamate and GABA. When these receptors are activated, patients tend to carry the feelings of relaxation and emotional balance with them after treatment.
- Balanced effects: When glutamate and GABA reach a stabilized baseline, the brain begins to grow new neural pathways. With this new growth, the patient suffering from deep depression may start to see measurable results.
Ketamine Trip Timeline
The effects of ketamine will vary based on the individual. Factors such as dosage, consumption method, personal body chemistry, and set and setting will play a large role in the experience. According to the National Institute on Drug Abuse (NIDA), “The effects of ketamine typically last 45 to 90 minutes depending on the dose. For some people, effects can last for several hours or even days.”
In general, there are experiences and physical symptoms with drug use that each user will encounter to varying degrees. From the comeup to the comedown of ketamine, let’s explore some common themes.
Phases of an Experience
When consumed intranasally, it takes approximately 15 minutes for the ketamine to take effect. When taken orally, it may take 20 minutes to an hour to feel the effects. During the ketamine comeup the user will start to feel relaxed, with any tension in the body starting to release. When used as an anesthetic, any pain will dissipate, and an overall calming effect will sink in.
At the peak of the ketamine trip, users will experience a trancelike state, accompanied by feelings of intense euphoria. Again, this experience is largely based on dosage. The threshold dose is about 0.3 mg per pound of body weight, with a light dose of 0.6 mg per pound of body weight. A range of 0.75–2 mg is considered a standard amount. This is where users often refer to the experience as a “warm blanket” enveloping them. A strong dose is somewhere between 1.5–2.5 mg per pound of body weight. At this dose, the ketamine can produce visual and auditory hallucinations.
When you enter the 3–4 mg per pound of bodyweight dosage, users enter the possibility of a “k-hole.” This is when users may feel as though they have left their bodies and are melting into their environment. Some describe this as similar to a near-death experience. The k-hole occurs when ketamine produces a coma-like state, which can be either exuberant and profound or terrifying and disturbing. Ketamine is a strange drug, in that even the slightest increase in dosage can take you from a fun body buzz to (temporary) body paralysis. During the ketamine comedown, there may be residual signs of lethargy, agitation, confusion, elevated blood pressure and dissociation.
Tips for How to Come Down From Ketamine
While there is nothing that can stop a ketamine trip in its tracks, you can lessen the effects of the ketamine comedown in a few key ways. Remember that the numbing effect associated with ketamine might prevent you from having full mobility, so be extra cautious when moving around so you do not trip or fall. Above all, trust that the effects will subside in a relatively short amount of time. In addition, it’s best to stay calm and focus on your breathing. In the event you find yourself having a bad trip, try the following suggestions.
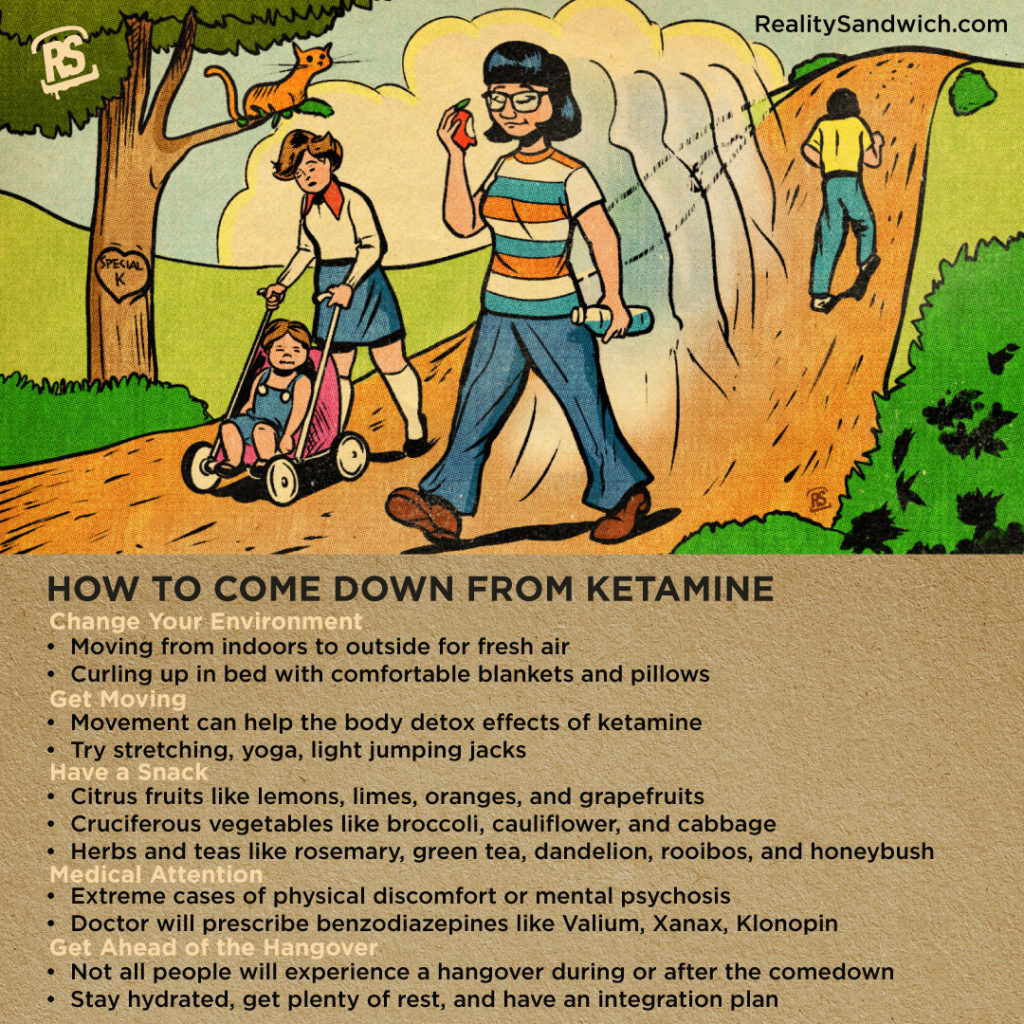
Change Your Environment
Hindsight is 20/20, as they say, but it’s worth mentioning that you should always consider set and setting before any psychedelic experience. Even so, once under the influence, it’s possible to find yourself not enjoying your environment. Therefore, make sure you have a plan in place to get from point A to point B. For example, if you are socially interacting somewhere, and feel the need to escape from the environment to process your thoughts and emotions, find a sober and trusted friend to get you home, or another safe place. Sometimes, a change in environment might be as simple as moving from indoors to outside for fresh air. It might also just mean curling up in bed with comfortable blankets and pillows to help integrate the experience as you come down.
Get Moving
Speeding up your metabolism through movement can help your body detox the effects of ketamine. This doesn’t necessarily mean going for a run. But even some light jumping jacks or yoga or meditation might help. Again, proceed with caution, as your body is in a sedative state, and you may not yet have full mobility. Start with stretching, and have a trusted trip sitter to help guide you in your decision-making.
Have a Snack
Enjoy a snack that promotes glucuronidation to help your body detox during the ketamine comedown. To support glucuronidation, eat citrus fruits like lemons, limes, oranges, and grapefruits. Cruciferous vegetables are also helpful, and herbs and teas like rosemary, green tea, dandelion, rooibos, and honeybush. A hot cup of green tea with honey and lemon would be an excellent choice.
Medical Attention
In extreme cases of physical discomfort or mental psychosis, you may wish to seek medical attention. Most commonly, if someone seeks medical attention in response to an unpleasant experience during the ketamine comedown, a doctor will prescribe benzodiazepines. These include Valium (diazepam), Xanax (alprazolam), Klonopin (clonazepam), or other drugs that treat anxiety disorders. Benzodiazepines can further settle the user down from the ketamine experience.
Get Ahead of the Hangover
Any drug use comes with potential risks, so you should always take advanced precautions. This includes not only preparing for the experience itself but the potential hangover that may come along with it. Although not all users will experience a hangover during or after the ketamine comedown, stay hydrated, get plenty of rest, and have an integration plan. It might be helpful to journal your experiences or have someone you trust that you can talk to about your experience. When used responsibly, ketamine can be a powerful tool. Above all, consider your health and overall condition, and seek professional advice whenever possible.
We want to hear from our community. Let us know in the comments below how you’ve handled a ketamine comedown in the past.
RS Contributing Author: Holly Crawford
Holly is a lover of the written word. She enjoys using language to tell stories about people, products, and ideas. With her roots deeply entrenched in the cannabis industry, she gravitates toward all things psychedelic with open-minded curiosity. If she isn’t musing in one of her journals, you can find her talking to her plants, studying business and spirituality, and performing all kinds of kitchen witchery. Holly lives in Oregon with her husband and their three dogs and two cats. You can follow her on Instagram @m_sungreen.